The term diabetes mellitus defines disorders of abnormal carbohydrate metabolism that are indicated by high blood sugar levels. It is associated with an absolute or relative impairment in insulin secretion, along with deviating degrees of peripheral resistance to the action of insulin.
Blood glucose is the direct energy source and comes from our food. Insulin enables glucose from food into your cells to be used for energy. Unfortunately, your body sometimes doesn’t make enough insulin or doesn’t employ insulin agreeably. Glucose then remains in the blood and doesn’t get into your cells. The hormone insulin drives sugar from the blood into your cells to be used or stored for energy.
An increase in Blood Pressure levels can cause damage to your eyes, nerves, kidneys, and other organs.
American Diabetes Association criteria for the diagnosis of Diabetes:
- Glycosylated hemoglobin A1C ≥6.5%. Fasting blood sugar after above ≥126 mg/dL (7 mmol/L). Fasting is defined as no caloric intake for at least 8 hours. OR
- 2-hour plasma glucose ≥200 mg/dL (11.1 mmol/L) during an Oral Glucose Tolerance Test.
- Classic symptoms of hyperglycemia or hyperglycemic crisis, random plasma glucose ≥200 mg/dL (11.1 mmol/L).
TYPES OF DIABETES:
Diagnosis for new-onset Diabetes in adults includes type 2 diabetes, type 1 diabetes, diseases of the exocrine pancreas, drug-induced Diabetes, and much rarer causes, such as maturity-onset Diabetes of the young (MODY). Type 2 diabetes accounts for over 90% of cases of Diabetes.
The following are the major types of Diabetes:
Type 1 Diabetes:
Type 1 diabetes mellitus, one of the most common chronic diseases in childhood, is caused by insulin deficiency following autoimmune destruction of the insulin-producing pancreatic beta cells. It most commonly presents in childhood, but one-fourth of cases are diagnosed in adults.
In genetically susceptible individuals, exposure to one or more environmental agents (e.g., viruses or foods) triggers an immune response that ultimately destroys the insulin-producing pancreatic beta cells. As a result, these patients require insulin for treatment. But, unfortunately, your body doesn’t make enough insulin.
Type 2 Diabetes:
Type 2 Diabetes is the most common form of Diabetes in adults accounting for more than 90% of cases, and is characterized by hyperglycemia and variable degrees of insulin resistance and deficiency. Its preponderance rises markedly with increasing degrees of obesity. Insulin deficiency and insulin resistance can arise through genetic or environmental influences, making it difficult to determine the actual cause in an individual patient. In addition, hyperglycemia itself can impair pancreatic beta cell function and exacerbate insulin resistance, called “glucotoxicity. So it is essential to maintain reasonable sugar control to prevent further pancreatic damage.
Gestational Diabetes:
Gestational Diabetes occurs when a woman’s insulin secretory capacity is not sufficient to overcome both the insulin resistance created by the anti-insulin hormones secreted by the placenta during pregnancy (e.g., estrogen, prolactin, human placental lactogen, cortisol, and progesterone) and the increased fuel consumption necessary to provide for the growing mother and fetus. It is estimated to occur in approximately 2.1 percent of pregnant women, usually developing in the second or third trimester. This type of Diabetes drops out after delivery. If you have had gestational Diabetes, you have a more significant chance of getting type 2 diabetes after that in life.
Other Types Of Diabetes:
- Genetic defects of pancreatic beta cell function or insulin secretion
- Diseases of the Pancreas like pancreatitis, Cystic fibrosis, hemochromatosis
- Endocrine disorders like Hyperthyroidism, Cushing’s syndrome, acromegaly, pheochromocytoma
- Drug-induced Diabetes is seen with Steroids, Beta-blockers, Thiazides, antipsychotics, some anti-epileptic medications, etc.
- Some infections leading to Diabetes are Rubella infection at birth, Cytomegalovirus infection.
- Genetic syndromes with Diabetes include Downs syndrome, Klinefelter’s syndrome, turner syndrome, Porphyria, myotonic dystrophy, etc. Less common types include monogenic Diabetes, inherited Diabetes, and cystic fibrosis-related Diabetes.
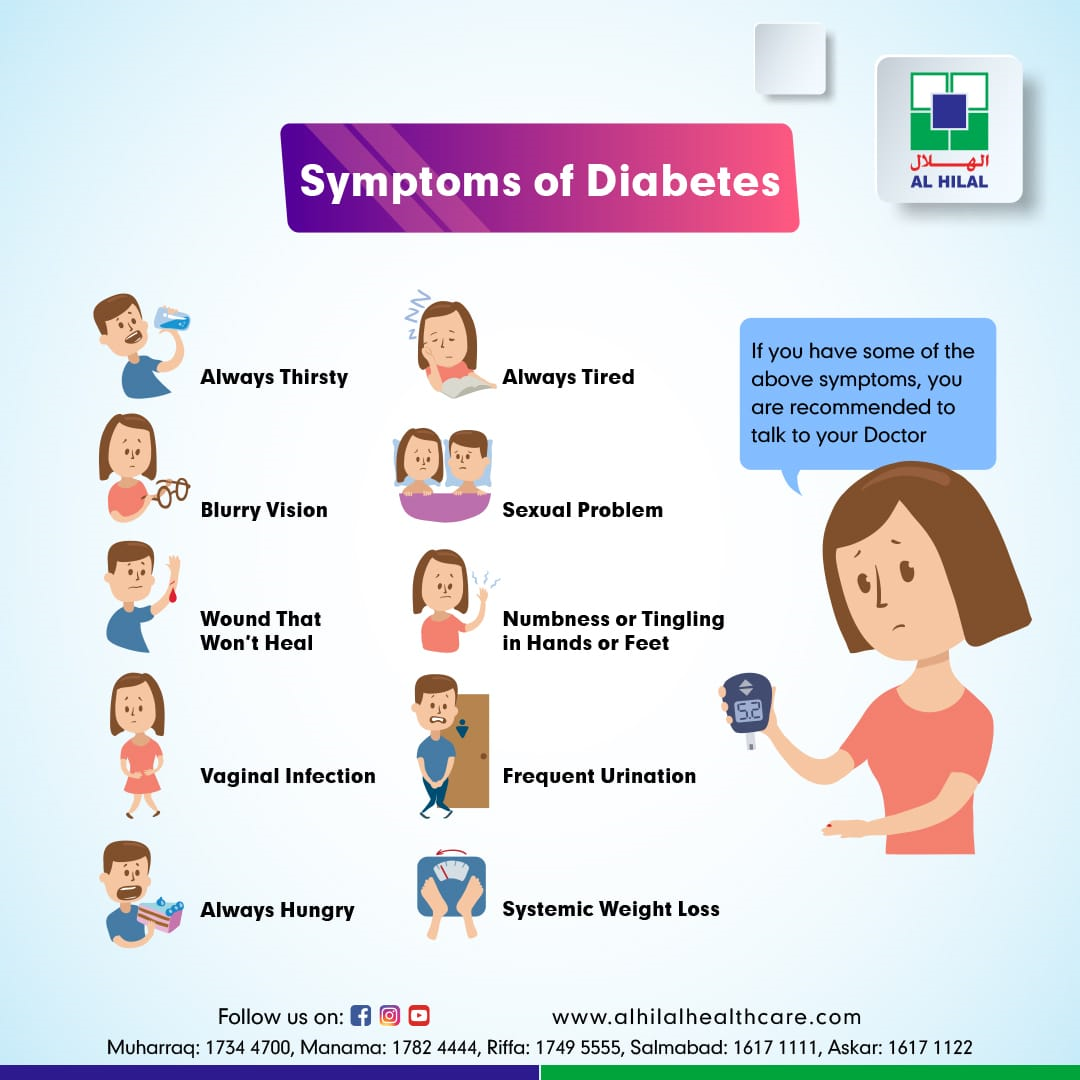
SYMPTOMS OF DIABETES:
- Diabetes can remain asymptomatic for years until complications develop
- Urinate a lot, often at night
- Increased thirst
- Abnormal loss of weight and loss of muscle mass
- Increased appetite
- Blurring of vision
- Numbness, tingling burning of hands or feet
- Tiredness
- Frequent Fungal infections of the skin and genitals
- Delayed healing of cuts and wounds
MAJOR COMPLICATIONS OF DIABETES:
Diabetes affects many organs adversely, leading to multiple diseases and decreasing quality of life and life span; uncontrolled Diabetes causes cardiovascular issues like Heart attack, stroke, kidney diseases and ultimately a failure, eye damage like retinopathy and cataract, Nerve diseases, Memory problems, hearing loss, erectile dysfunction, depression, skin infections, and dental issues are the significant complications of Diabetes.
But many of these can be prevented by proper treatment of Diabetes. As evidenced by landmark studies in Diabetes, each 1% reduction in mean HbA1cwas associated with a 21%reduction in risk of any end point related to Diabetes,21% for deaths associated with Diabetes, 14% for Heart attack, and 37% for microvascular complications. Otherwards each 1 % higher HBa1c from average increases your risk of developing heart attack by 14% and risk of other complications by 37 %. These can be prevented by proper control of blood sugar by diet, exercise, and medications prescribed by your doctor.
PREVENTION OF TYPE 2 DIABETES MELLITUS:
The goals of diabetes prevention include:
- Preventing or delaying the onset of Diabetes
- Preserving beta cell function
- Preventing or delaying microvascular and cardiovascular complications
- Ultimately, reducing costs of diabetes care
- Exercise — Although there is no one exercise prescription for all individuals, adults at high risk for Diabetes are encouraged to perform 30 to 60 minutes of moderate-intensity aerobic activity on most days of the week (at least 150 minutes of moderate-intensity aerobic exercise per week).
- Diet — Choosing a dietary pattern of healthful foods, such as the Dietary Approaches to Stop Hypertension (DASH) or Mediterranean-style Diet, rather than focusing on a specific nutrient. This approach allows greater flexibility and personal preference in diet and may improve long-term adherence. Mediterranean Diet appeared to reduce the incidence of Diabetes independent of weight loss.
- Smoking —Smoking cessation may reduce diabetes risk by reducing systemic inflammation.
- The weight control can prevent or delay Diabetes by losing 5 to 10% of your current weight if your BMI is above 25.
TREATMENT OF DIABETES:
Type 1 diabetes needs Insulin injections as primary treatment. Insulin can be administered either by injections or by using an insulin pump.
The cornerstone in managing Type 2 diabetes is proper diet and exercise. Other treatment options complement diet and exercise. Various treatment options are available. Depending on case to case, it varies from diet and exercises alone, oral medications, Insulinor Injectable GLP-1, or even in some cases of Morbid obesity, bariatric surgery depending upon other co-morbidities.
Your treatment options may differ if you have another type of Diabetes.


