January is the month of Cevical cancer awareness. Its critical to highlight the importance of cervical cancer screening to all women of reproductive ages. About 600,000 women battle cervical cancer every year. Its ranked as 4 th most common cancer among women, and it is more easily treatable, if diagnosed early. Women with Cervical cancer hava a long asymptomatic period before it become clinically symptomatic and evident.
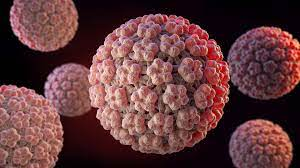
Human Papilloma Virus (HPV), a double stranded DNA virus, is the most common viral infection that affects teens and adults and it is responsible for cervical cancers and mortality. The prevalance of HPV in young adult females can range between 30-80%. The life time probability of ever encountering HPV is as high as 80-90%. HPV can lead to 6 types of deadly cancers includign cancer of the cervix, Vulva, Vagina, Penis anus and back of throat
Approximate 200 types of HPV have been characterized out of which 16, 18, 31, 33, 35, 45, 52, and 58 cause cancers. Cervical cancer is commonest in women while the oropharyngeal cancer in men
How is HPV acquired?
HPV infection can be a normal part of becoming a sexually active adult. It can be passed on at the first sexual debut- and it is not a result of sexual promiscuity. HPV is transmitted through contact with mucous membranes, body fluids including oral & anal sex. 90% of HPV infections are cleared with natural body immunity.
Risk factors and predisposing conditions for invasive cancer are high risk HPV types, immunocompromised status, co-infection with Sexually Transmitted Infections (STI), homosexuals, smoking, multiple sexual partners etc.
One can not get HPV by hugging, holding hands, sharing swimming pool, hot tubs, sharing food, toilet seats. Most of HPV-associated cancer lesions remain asymptomatic. Condoms give some protection against HPV but not completely.
Pathophysiological aspects
The positive part related with HPV-induced cancers is that, it takes long time to develop into cancer (15-20 years in immune and 5-10 years in immunocompromised (as HIV infected) cases. Atypical cellular changes can be detected easily from mucous scrapes (surface biopsy – pap smear ) or HPV genotyping and timely treatment can prevent cancers.
Having a positive HPV test does not mean you have cervical cancer or you will get cancer in future. It only means that you have a high risk strain which ony needs to be followed up closely. There is no treatment for HPV, but in most cases it goes away without treatment.
Prevention
Another good aspect in relation to HPV is that we have both the prevention at all levels; primarily by vaccines (bivalent, quadrivalent and nanovalent) and then by cervical screening. WHO on 17th November 2020 launched the global strategy of cancer elimination that included the ‘90-70-90’ triple intervention targets to be met by 2030 i.e., 90% girls be vaccinated by the age of 15 years, 70% women up to 45 years of age be screened and 90% of affected women (pre-cancerous or cancer) be managed. This is an ambitious time – line to reach the target and we have just 7 years. And this can be acheived with colloboration and team work from all nations
HPV vaccination

HPV Vaccines are safe and effective in preventing HPV infection, precancerous lesions and Invasive cancers. Vaccinating girls aged 9-14 could prevent 40% of cervical cancer deaths before 2030
- Routine vaccination is recommended at 11-12 years, while catch up vaccination up to 26 years can be done.
- From 27-45 years it should be based on shared clinical decision making with counselling that it may not affect if HPV strains have already infected.
- 2-dose schedule is enough before 15 years (0 & 6-12 month) and after that 3-dose schedule is recommended as 0 (baseline), 1 (1-2 month) 6 (6 month).
HPV screening and Pap Test
In the recent past, women were advised to visit their ob-gyn every year for a Pap test, as well as a pelvic exam and breast exam. The Pap smear, is a screening test for cervical cancer.
Today, and our advice has changed. Women should still visit their ob-gyn each year,but we no longer advise women to have an annual Pap test. A big reason for the change: We now better understand the way cervical cancer develops over time—we know it takes many years to develop—so we’ve expanded the time between screenings.
We also now have two screening options to detect cervical cancer, the Pap test and the HPV test. With both tests, cells are taken from the cervix and tested. The Pap test looks for abnormal cells that may develop into cancerous cells over time. The HPV test looks for the strains of HPV that are most likely to cause cancer. HPV genotype as primary screening tool is recommended test now. Ideally co-test or HPV genotype every 5 years is recommended strategy but pap smear every 3 years is also considered optimal.
In areas with limited resources, the visual inspection (VI) & with acetic acid (VIA) is done

ACOG guidelines for cervical cancer screening
-
- Women age 21 to 29 should have a Pap test alone every 3 years.
- Women age 30 to 65 have three options for testing. They can have both a Pap test and an HPV test every 5 years. They can have a Pap test alone every 3 years. Or they can have HPV testing alone every 5 years.
- After age 65, you can stop having cervical cancer screenings if you have never had abnormal cervical cells or cervical cancer, and you’ve had two or three negative screening tests in a row, depending on the type of test.
If you have more question on Cervical cancer and HPV Vaccination, please reach the author, Dr.Krishna Kavita Ramavath MD MRCOG(UK), FACOG(USA) at Al Hilal Manama. She is Internationally trained, Specialist OBGYN and Gyne Oncologist- available 1pm- 9pm daily Tuesday to Sunday. Friday 9pm-5pm


